 HISTORY: ABNORMAL ECHOCARDIOGRAM
HISTORY: ABNORMAL ECHOCARDIOGRAM
COMPARISON: None
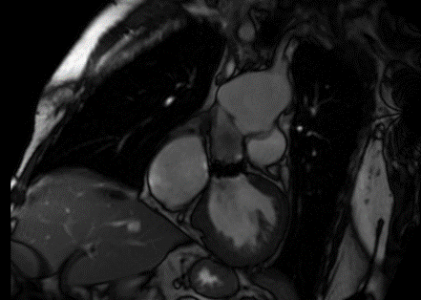
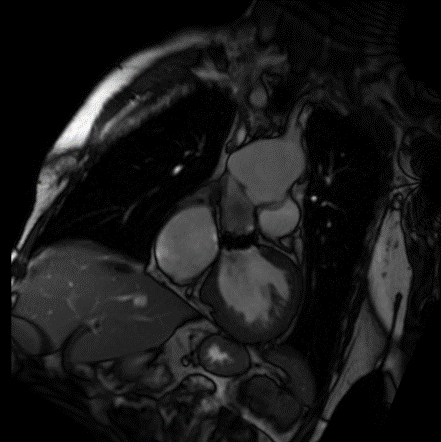
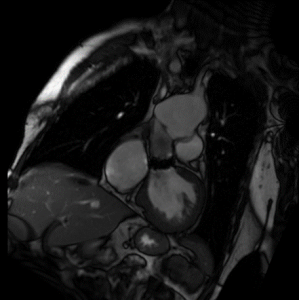
TECHNIQUE: Multiplanar images of the heart were obtained at 1.5 Tesla. Morphologic and dynamic cine imaging was performed in multiple projections. 19 mL of intravenous Gadavist was administered for delayed enhancement imaging. Flow quantification sequences were obtained. Post processing included flow and volume calculations, which were performed by the interpreting physicians on an independent workstation.
FINDINGS:
Thoracic aorta: the patient is status post median sternotomy and graft replacement of the aortic root and aortic valve replacement. There is aneurysmal dilation of the distal thoracic aorta, just proximal to the aortic arch, measuring 6.7 cm in diameter. There is a septation within the aortic lumen, at the anastomosis of the graft and distal ascending thoracic aorta.
Pulmonary artery: the main pulmonary artery is dilated, measuring 3.9 cm in diameter.
Systemic and pulmonary venous return: Conventional
Interatrial septum: Intact
Cardiac chambers: Normal atrioventricular and ventriculo-arterial concordance.
Coronary arteries: Normal origins
Left ventricle: the left ventricular size is moderately enlarged. Left ventricular systolic function is severely depressed. At the base of the heart the anterior wall is akinetic. At the mid-level, the anterior septum, anterior wall, and anterolateral wall are akinetic. The entire apex is akinetic. The remainder of the heart is hypokinetic. There is relative hypertrophy involving the septum and lateral and inferior walls at the base and mid heart, with atrophy of the anterior wall and apex. T2 weighted imaging demonstrates no high signal intensity to suggest the presence of myocardial edema. Postcontrast images demonstrate transmural delayed myocardial enhancement throughout the anterior wall, with additional enhancement in the septum and lateral wall of the mid hearts and enhancement throughout the apex, consistent with infarction. No thrombus is visible in the left ventricle. There is no systolic anterior motion of the mitral valve or outflow tract obstruction.
LV MEASUREMENTS: quantification of the left and right heart volumes and function is significantly limited because of patient motion artifact and suboptimal breath hold cooperation.
BSA 2:21 sq. m., weight: 200 lb., height: 73 in
LVEDV: 229 ML: LVEDVI 131 ML/SQ M (Normal 95, mildly increased 95 – 115; moderately increased 116 – 135; severely increased > than 135 ml/sq m)
LVESV 273 ml LVESVI 123 ml/sq m
LVSV: 16.3 ml LVSVI 7.4 ml/sq m
LVEF: 10% (Normal 55-78%, mildly depressed 40-54%, moderately depressed 30-39%, severely depressed 30%)
EDD: 58 mm (normal 43 – 59 mm)
ESD: 54 mm (normal 26 – 40 mm)
Anterior septal wall: 18 mm (normal 12 mm)
Posterior septal wall: 12 mm (normal 11 mm)
LV mass: 190 g
LV mass index: 86 g/sq m (Normal 80, mildly increased 81 – 99, moderately increased 100 – 120, severely Inc. increased > 120 g/sq m)
Cardiac output: 2.5 L/min
Cardiac index: 1.12 L/min/sq m
Right ventricle: the right ventricular size is normal. Right ventricular systolic function is globally severely depressed. No segmental wall motion abnormalities or aneurysms are seen postcontrast images demonstrate no delayed myocardial enhancement. No thrombus is visible in the right ventricle.
RV MEASUREMENTS:
RVEDV 190 ml RVEDVI: 86 ml/sq m (Normal 58 – 114, mildly increased 115 – 171, moderately increased 172 – 228, severely increased > 228 ml/sq m)
RVESV 165 ml RVESVI 75 ml/sq m
RVSV 25 ml RVSVI 1.1 ml/sq m
RVEF 13% (Normal >46%, mildly depressed 36 – 46%, moderately depressed 25 – 35%, severely depressed 25%)
Left atrium: the left atrial size is moderately enlarged, measuring 5.6 cm AP in end systole (Normal 3.1 – 4.3) no thrombus is visible in the left atrium.
Right atrium: the right atrial size is mildly enlarged, measuring 5.3 cm AP in end systole on the four – chamber view (Normal 3.0 – 4.5). No thrombus is visible in the right atrium
Aortic valve: there is a mechanical valve in the aortic position. There is a mild degree of aortic regurgitation. Phase – contrast imaging at the ascending aorta reveals a forward flow of 85 cc/heartbeat.
Pulmonic valve: there is no significant pulmonic stenosis or regurgitation. Phase – contrast imaging at the main pulmonary artery reveals a forward flow of 67 cc/heart beat.
Qp/Qs: Normal
Mitral valve: there is no significant mitral stenosis or regurgitation
Tricuspid valve: there is no significant tricuspid stenosis or regurgitation
Pericardium: No pericardial thickening, enhancement, or pericardial effusion is identified.
Lungs and pleura: No pleural effusions. Limited evaluation of the lungs demonstrates no abnormal signal characteristics.
Visualized upper abdominal organs: unremarkable.
IMPRESSION:
Moderately enlarged left ventricular chamber size, was severely depressed systolic function. Estimation of ejection fraction is limited as noted above, but probably less than 20%. There is underlying hypertrophic cardiomyopathy, with infarcts throughout the LAD and circumflex territories, resulting in relative atrophy of the anterior wall and cardiac apex.
Normal right ventricular chamber size with severely depressed systolic function. Moderately enlarged left atrium and mildly enlarged right atrium. No atrial thrombus.
Mechanical valve in aortic position, with mild aortic regurgitation.
Relatively normal appearance of the mitral, tricuspid, and pulmonic valves.
The main pulmonary artery is dilated, suggestive of pulmonary arterial hypertension.
Status post median sternotomy and graft replacement of the proximal ascending thoracic aorta, with persistent 6.7 cm aneurysmal dilation of the distal ascending thoracic aorta, just proximal to the aortic arch. There is a septation within the aortic lumen at the distal graft anastomosis.