Table of Contents
What conditions can an ophthalmologist diagnose with an MRI?
Magnetic Resonance Imaging (MRI) is a powerful diagnostic tool that has revolutionized the field of medicine, including ophthalmology. An MRI uses a magnetic field and computer-generated radio waves to create detailed images of the organs and tissues in the body. For ophthalmologists, this technology is instrumental in diagnosing a range of conditions affecting the eyes and the surrounding structures with high precision.
Specific Magnetic Resonance Exams Used for Ophthalmology
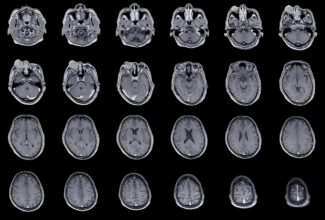
Magnetic Resonance Imaging – MRI of the Brain
MRI of the Brain plays a critical role in diagnosing and managing various ophthalmic conditions by providing detailed images of the brain’s structures. MRI of the brain is a non-invasive procedure that does not involve radiation, making it safe for repeated use in monitoring disease progression or the effectiveness of treatment in these conditions. It is a versatile tool that, depending on the specific sequences used, can provide invaluable insights into a wide range of ophthalmic and neurological conditions, guiding diagnosis, treatment, and prognosis.
Magnetic Resonance Imaging – MRI of the Face, Orbit, and Neck
MRI of the Face, Orbit, and Neck is a comprehensive imaging approach that provides detailed views of the facial structures, eye orbits, and neck. This wide-ranging perspective is particularly valuable in diagnosing and managing ophthalmic conditions that may involve not just the eyes themselves but also the surrounding tissues, the orbital structure, and even the pathways that might affect vision or eye health indirectly through the neck. MRI of the face, orbit, and neck offers a non-invasive, detailed examination method without the use of ionizing radiation, making it particularly well-suited for diagnostic evaluations where a comprehensive view of the anatomy is necessary.
Magnetic Resonance Venography (MRV)
MRV is a specialized MRI technique focused on visualizing the veins. It provides detailed images of the venous systems within the body, including those in the head and neck, using magnetic fields and radio waves. MRV is particularly useful for assessing venous blood flow and detecting abnormalities such as thrombosis (blood clots), stenosis (narrowing of the veins), or malformations.
The technique for MRV usually involves the use of a contrast agent to enhance the visibility of the veins, although non-contrast techniques are also available and can be particularly useful in patients who have contraindications to contrast media. The choice between contrast-enhanced and non-contrast MRV will depend on the specific clinical scenario and patient factors. MRV’s ability to provide detailed images of the venous system without ionizing radiation makes it an essential tool in the diagnostic workup of certain ophthalmic conditions, especially when venous pathology is suspected. It complements other imaging modalities by offering unique insights into the venous structures that could affect or be affected by ophthalmic diseases.
Magnetic Resonance Angiography (MRA) of the Head
MRA is a specialized MRI technique designed to visualize the blood vessels in the brain without the need for catheters or radiation. It uses a powerful magnetic field and pulses of radio wave energy to generate detailed images of the arteries and veins. In the context of ophthalmic diseases, MRA can be particularly useful for diagnosing conditions where the blood supply to the eye and optic nerve is affected or where vascular abnormalities contribute to the disease process.
MRA is a non-invasive, relatively quick procedure that does not require the use of iodinated contrast agents, making it a safer choice for patients with kidney problems or allergies to contrast dyes. However, it’s worth noting that while MRA is highly effective for visualizing blood vessels, it is typically used as a complementary technique alongside other imaging modalities, depending on the specific needs of the diagnosis and treatment plan for ophthalmic conditions.
Specific Ophthalmic Conditions and Diagnostic Tests, Including MRI used by Ophthalmologists
Strabismus
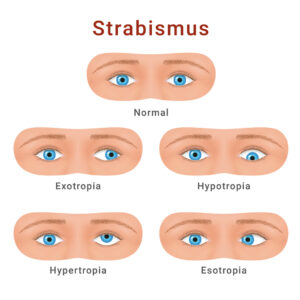
This condition involves a misalignment of the eyes, where they do not look at the same point at the same time. MRI can help in identifying the underlying causes, such as abnormalities in the eye muscles, nerves, or brain areas responsible for eye movement control.
- Comprehensive Eye Examination: Evaluates vision, eye health, and the extent of eye misalignment.
- Cover Test: Identifies whether strabismus is constant or intermittent and which eye is affected.
- Light Reflex Test: Detects misalignment by observing light reflection on the corneas.
- Prism Test (Prism Adaptation Test): Measures the degree of eye turn for treatment planning.
- Ophthalmoscopy and Slit-Lamp Exam: Checks internal and external eye structures to exclude other issues.
- Stereopsis Test: Assesses the ability to perceive depth, which strabismus can impair.
- Refraction: Determines refractive errors that may contribute to strabismus, aiding in correction.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head, and MRI face/orbit/neck exams.
Age-Related Macular Degeneration (AMD)
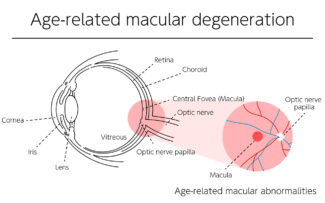
AMD is a primary cause of vision impairment in people over 50, primarily affecting the macula, which is crucial for central vision tasks such as reading, driving, and facial recognition. AMD exists in two forms: dry (atrophic) and wet (neovascular or exudative). Diagnosis is centered on a thorough assessment of the patient’s ocular history, presenting visual symptoms, and specialized retinal tests.
- Comprehensive Eye Examination: Assesses visual acuity and identifies any initial signs of vision loss.
- Dilated Eye Exam: Utilizes pupil dilation to examine the retina and macula, looking for signs like drusen and pigmentation changes.
- Amsler Grid Test: Helps detect macular changes by revealing any distortions in straight lines on a grid pattern.
- Optical Coherence Tomography (OCT): Offers detailed images of the retina, revealing changes consistent with AMD, such as retinal thinning, thickening, or swelling.
- Fundus Autofluorescence (FAF): Provides insights into the health of the retinal pigment epithelium, detecting areas of atrophy relevant to AMD progression.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams.
Ocular and Orbital Tumors
MRI is highly effective in identifying and characterizing tumors within the eye (ocular) or in the orbit, the cavity that contains the eye. It provides detailed images that help in determining the size, location, and impact of tumors on surrounding structures.
- Comprehensive Eye Examination: Evaluates visual acuity, eye movements, pupil responses, and visible abnormalities to detect signs of tumors.
- Slit-Lamp Examination: Offers a magnified, three-dimensional view of the eye’s interior, crucial for identifying intraocular tumors like uveal melanoma or retinoblastoma.
- Ophthalmoscopy: Allows detailed inspection of the retina and optic nerve, essential for spotting intraocular tumors.
- Ultrasound (B-scan): Non-invasive method for assessing the internal structure of the eye and orbit, distinguishing between solid and cystic masses.
- Biopsy: Sometimes necessary for a definitive diagnosis, involving tissue sample examination under a microscope. The biopsy method depends on the tumor’s location and characteristics.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams.
Amblyopia (Lazy Eye)
Amblyopia is a vision development disorder where an eye fails to achieve normal visual acuity, even with prescription eyeglasses or contact lenses. MRI can aid in identifying structural abnormalities of the eye or brain that may contribute to amblyopia.
- Visual Acuity Test: Assesses clarity of vision in each eye, often using a Snellen chart or a picture chart for children.
- Refractive Error Assessment: Determines the degree of nearsightedness, farsightedness, or astigmatism in each eye using methods like retinoscopy.
- Ocular Health Examination: Explores the overall health of the eye’s internal and external structures to exclude other causes of vision impairment.
- Cover Test: Evaluates eye alignment and cooperation by covering each eye alternately while focusing on a distant object.
- Stereopsis (Depth Perception) Test: Measures the binocular ability to perceive depth, which can be impaired in amblyopia.
- Other Diagnostic Tests: Additional specialized tests may be conducted if physical obstructions like cataracts are suspected.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head, and MRI face/orbit/neck exams.
Glaucoma
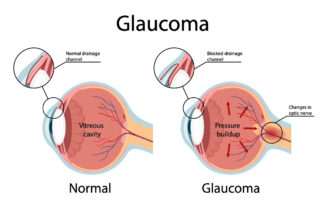
Primarily diagnosed through clinical tests assessing eye pressure, visual field, and optic nerve damage, MRI can be used for advanced glaucoma cases to assess optic nerve damage and to rule out any neurological causes behind the condition.
- Tonometry: Measures IOP to identify elevated pressure levels, utilizing instruments like the Goldmann applanation tonometer.
- Ophthalmoscopy (Dilated Eye Exam): After pupil dilation, the optic nerve is examined for damage using a magnifying lens, indicative of glaucoma.
- Visual Field Test (Perimetry): Assesses peripheral vision loss through a machine test, crucial for mapping the extent of vision impairment and monitoring progression.
- Pachymetry: Non-invasive measurement of corneal thickness, important as thin corneas can elevate glaucoma risk and affect pressure readings.
- Gonioscopy: Evaluates the eye’s drainage angle to distinguish between open-angle and angle-closure glaucoma, guiding treatment decisions.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head, and MRI face/orbit/neck exams.
Drusen of the Optic Disc
These are yellow deposits under the retina or on the optic nerve head. MRI can help in differentiating optic disc drusen from other conditions like papilledema, providing clarity on the diagnosis.
- Ophthalmoscopy: Enables the visualization of the optic disc, revealing superficial drusen as refractile bodies, while buried drusen may mimic disc swelling.
- Ultrasound (B-scan): Essential for identifying buried drusen, which appear as highly reflective regions with acoustic shadowing.
- Fundus Autofluorescence: Helps visualize drusen by highlighting their hyper-autofluorescent nature due to calcium content, differentiating them from other disc anomalies.
- Visual Field Testing: Identifies visual field defects associated with ODD, including blind spot enlargement or peripheral field loss, through standard automated perimetry.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams.
Albinism (Structural Abnormalities)
Albinism is a group of genetic conditions characterized by a lack of melanin pigment in the eyes, skin, and hair. MRI can visualize structural abnormalities in the eye and visual pathways that are associated with the condition.
- Visual Acuity Testing: Determines the clarity of vision, which is often impaired in albinism.
- Ophthalmoscopy: Reveals the retina’s pigmentation level and any structural irregularities.
- Slit Lamp Examination: Detects iris transillumination defects through detailed iris observation.
- Optical Coherence Tomography (OCT): Offers precise retinal images to identify foveal hypoplasia.
- Visual Field Testing: Evaluates peripheral vision for any significant visual field deficits.
- MRI Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams.
Diplopia (Double Vision)

Diplopia can result from a range of causes, including nerve damage and muscle weakness. MRI can help in identifying the cause of diplopia by providing images of the eye muscles, nerves, and brain.
- Patient History: Collects details on the onset, consistency, and any symptoms accompanying the double vision.
- Visual Acuity Test: Assesses the clarity of vision in each eye.
- Cover Test: Determines eye alignment by observing eye movements as one eye is covered and then uncovered.
- Ocular Motility Test: Evaluates the range and strength of eye movements.
- Pupillary Light Reflex Test: Checks the pupils’ reaction to light for nerve or internal eye damage.
- Prism Test: Measures the degree of eye misalignment by identifying the amount of prism needed to merge the images into one.
- Slit-Lamp Examination: Inspects the front part of the eye for abnormalities that could cause monocular diplopia.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams.
Optic Neuritis
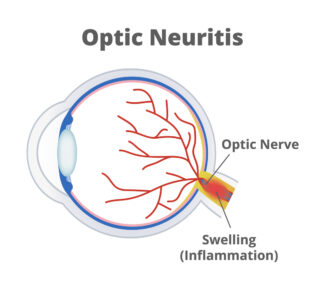
This is an inflammation of the optic nerve that can cause sudden loss of vision or blurred vision in one eye. MRI is used to visualize the inflammation and to check for possible underlying causes, such as multiple sclerosis.
- Clinical History and Symptom Assessment: Involves a thorough examination of symptoms such as the onset of vision loss, eye pain, visual phenomena (photopsias), and changes in color perception.
- Visual Acuity Test: Measures the clarity of vision, which may be impaired in the affected eye.
- Pupillary Light Reaction Test: The swinging flashlight test can detect a relative afferent pupillary defect (RAPD), indicating compromised optic nerve function.
- Color Vision Testing: Identifies color vision impairments, with optic neuritis possibly dulling color intensity.
- Visual Field Testing: Maps peripheral vision to pinpoint characteristic vision loss patterns associated with optic neuritis.
- Ophthalmoscopy: Checks the optic disc for swelling or abnormalities, noting that the optic disc may look normal initially in cases of retrobulbar optic neuritis.
- Optical Coherence Tomography (OCT): Provides detailed retina and optic nerve imagery, useful for gauging retinal nerve fiber layer thickness, which might decrease after optic neuritis.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams.
Pseudotumor Cerebri

Also known as Idiopathic Intracranial Hypertension, this condition mimics brain tumors’ symptoms without an actual tumor being present. MRI can be crucial in ruling out actual brain tumors and assessing the effects of increased brain pressure on the optic nerves.
- Medical History and Physical Examination: Focuses on assessing symptoms and medical background, with specific attention to visual symptoms and the detection of papilledema, indicative of increased ICP.
- Ophthalmologic Evaluation: Conducted by an eye specialist to examine the eyes for papilledema and perform visual field tests to identify any vision loss or blind spots, key indicators of the condition.
- Brain Imaging Tests (MRI or CT scans): Essential for excluding other causes of symptoms, such as brain tumors, venous sinus thrombosis, or hydrocephalus. While typically normal in PTC cases, these scans are crucial for ruling out differential diagnoses.
- Venography: Utilized in certain instances to assess the cerebral venous sinus anatomy, MR venography or conventional venography helps identify venous sinus stenosis or thrombosis, conditions that can present similarly to or exacerbate PTC.
- MR Exams Typically Ordered Include: MRI Brain, MRA Head and MRI face/orbit/neck exams and MRV of the head.
In summary, MRI serves as a critical diagnostic tool in ophthalmology, offering non-invasive, detailed imaging that aids in the accurate diagnosis and management of various eye and orbital conditions. Its ability to visualize soft tissues with high resolution makes it indispensable for diagnosing complex conditions, assessing the extent of diseases, and planning treatment strategies. Follow these tips to maintain healthy eyesight, which is important to prevent blindness in children and adults.
GWIC offers MR imaging services that are instrumental in diagnosing and treating a variety of ophthalmic conditions. See your eye doctor regularly and report any changes in your vision.