Orthopedic MRI of the Knee: A Comprehensive Guide
Table of Contents
Overview of Knee MRI in Orthopedics
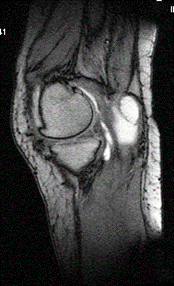
Magnetic Resonance Imaging (MRI) has revolutionized the field of orthopedic diagnostics, particularly in evaluating knee pathologies. The knee joint is one of the most complex and heavily utilized joints in the human body, making it susceptible to a wide range of injuries and degenerative conditions. MRI provides detailed images of the knee’s intricate structures—including bones, ligaments, tendons, cartilage, and menisci—without the use of ionizing radiation. This non-invasive imaging modality has become essential for accurate diagnosis, treatment planning, and monitoring of knee disorders.
This guide is designed to offer a comprehensive understanding of knee MRI for healthcare professionals, including radiologists, orthopedic surgeons, physical therapists, and medical students. It covers the fundamental anatomy of the knee, indications for MRI, technical aspects of MRI procedures, and interpretation of imaging findings. By consolidating key information and best practices, this guide aims to enhance diagnostic accuracy and improve patient outcomes.
Anatomy of the Knee
 Bones and Joints
Bones and Joints
The knee joint is a hinge-type synovial joint formed by three primary bones:
- Femur (Thighbone): The distal end articulates with the tibia and patella.
- Tibia (Shinbone): The proximal end supports the femur and bears weight.
- Patella (Kneecap): A sesamoid bone embedded within the quadriceps tendon.
The joint includes two main articulations:
- Tibiofemoral Joint: Between the tibia and femur.
- Patellofemoral Joint: Between the patella and femur.
These articulations allow for flexion, extension, and slight rotational movements essential for locomotion.
Ligaments
Ligaments provide stability by connecting bones and limiting excessive movement:
- Anterior Cruciate Ligament (ACL): Prevents anterior displacement of the tibia.
- Posterior Cruciate Ligament (PCL): Prevents posterior displacement of the tibia.
- Medial Collateral Ligament (MCL): Stabilizes the inner knee.
- Lateral Collateral Ligament (LCL): Stabilizes the outer knee.
These ligaments are critical in maintaining knee stability during dynamic activities.
Menisci
The menisci are two crescent-shaped fibrocartilaginous structures:
- Medial Meniscus: Larger and less mobile, attached to the MCL.
- Lateral Meniscus: More circular and mobile.
They function to:
- Distribute weight and reduce stress on articular cartilage.
- Provide shock absorption.
- Enhance joint stability.
 Tendons and Muscles
Tendons and Muscles
Key tendons and muscles include:
- Quadriceps Tendon: Connects the quadriceps muscles to the patella.
- Patellar Tendon (Ligament): Connects the patella to the tibial tuberosity.
- Hamstring Muscles: Involved in knee flexion and hip extension.
These structures are vital for knee movement and are common sites of injury.
Cartilage and Synovial Membrane
- Articular Cartilage: Smooth tissue covering bone ends, facilitating low-friction movement.
- Synovial Membrane: Lines the joint capsule, producing synovial fluid for lubrication.
Damage to cartilage can lead to osteoarthritis, while synovial inflammation can cause pain and swelling.
Indications for Knee MRI
Traumatic Injuries
MRI is the preferred imaging modality for assessing acute knee injuries:
- Ligament Tears: Particularly ACL and PCL injuries common in athletes.
- Meniscal Tears: Resulting from twisting injuries or degeneration.
- Occult Fractures: Not visible on X-rays but detected through bone marrow edema patterns.
Degenerative Conditions
Chronic conditions that benefit from MRI evaluation:
- Osteoarthritis: Assessment of cartilage loss, osteophytes, and subchondral changes.
- Cartilage Degradation: Early detection of chondral lesions before radiographic changes occur.
Inflammatory and Infectious Disorders
MRI helps diagnose:
- Synovitis: Inflammation of the synovial membrane, often in rheumatoid arthritis.
- Septic Arthritis: Infection within the joint, requiring prompt treatment.
Tumors and Cysts
Detection and characterization of:
- Benign Lesions: Such as ganglion cysts and Baker’s cysts.
- Malignant Tumors: Early identification of bone or soft tissue sarcomas.
Pre- and Post-Surgical Evaluation
MRI assists in:
- Surgical Planning: Providing detailed anatomy for procedures like ligament reconstruction.
- Post-operative Assessment: Evaluating graft integrity and detecting complications.
MRI Techniques and Protocols for the Knee
MRI Equipment and Settings

- Magnet Strength: A 1.5 Tesla MRI scanner is commonly used, offering a balance between image quality and patient accessibility.
- Coil Selection: Dedicated knee coils improve signal-to-noise ratio and image resolution.
Patient Preparation and Positioning
- Positioning: The patient lies supine with the knee placed in the coil, often slightly flexed (15-20 degrees) to reduce joint effusion artifacts.
MRI Sequences Used in Knee Imaging
Common sequences include:
- T1-Weighted Sequences: Provide excellent anatomical detail of fat-containing structures.
- T2-Weighted Sequences: Highlight fluid, making them useful for detecting edema and effusions.
- Proton Density (PD) Sequences: Offer high-resolution images of cartilage and menisci.
- Fat Suppression Techniques:
- Short Tau Inversion Recovery (STIR): Suppresses fat signals to detect edema.
- Fat-Saturated T2-Weighted Images (FatSat): Enhance visualization of fluid and pathology.
Use of Contrast Agents
- When Indicated: Contrast-enhanced MRI is used for detecting synovial disease, infections, or tumors.
- Gadolinium-Based Agents: Administered intravenously; generally safe but used cautiously in patients with renal impairment.
Advanced Imaging Techniques
- 3D Imaging: Allows multiplanar reconstructions from a single acquisition, improving anatomical assessment.
- Diffusion-Weighted Imaging (DWI): May help in tumor characterization and detecting bone marrow lesions.
Interpretation of Knee MRI
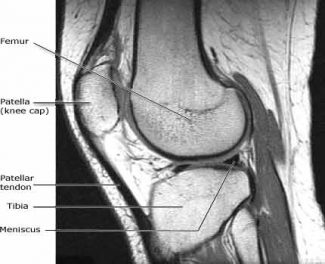
Normal MRI Anatomy
Recognizing normal structures is essential:
- Bones: Should show normal marrow signal without lesions.
- Ligaments: Appear as low-signal-intensity bands; intact fibers indicate normalcy.
- Menisci: Triangular low-signal structures between femoral condyles and tibial plateau.
- Cartilage: Smooth, continuous high-signal layer on T2-weighted images.
- Synovial Fluid: Normally minimal; increased fluid suggests effusion.
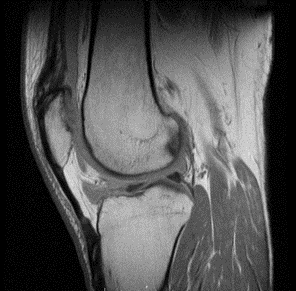
Pathological Findings
Ligament Injuries
- ACL Tears: Disruption or increased signal intensity within the ligament.
- PCL Tears: Less common; may show partial or complete disruption.
- Collateral Ligament Injuries: Swelling and increased signal on T2-weighted images.
Meniscal Tears
Types of tears:
- Horizontal: Parallel to the tibial plateau; may form meniscal cysts.
- Vertical Longitudinal: Perpendicular to the tibial plateau; can lead to “bucket-handle” tears.
- Radial: Extends from the free edge towards the periphery; disrupts hoop stress function.
Cartilage Defects
- Chondral Lesions: Graded I-IV based on depth and severity; important in osteoarthritis.
- Osteochondral Lesions: Involve both cartilage and underlying bone.
Bone Marrow Edema
- Appearance: Increased signal on fluid-sensitive sequences.
- Causes: Trauma, osteoarthritis, insufficiency fractures.
Synovial Disorders
- Synovitis: Thickened synovial membrane with enhancement after contrast administration.
- Pigmented Villonodular Synovitis (PVNS): Low-signal intensity due to hemosiderin deposition.
Tumors and Cysts
- Baker’s Cyst: Fluid-filled sac located posteriorly; communicates with the joint space.
- Tumors: Characterized by their signal intensity, enhancement patterns, and effects on adjacent structures.
Reporting Standards
A comprehensive MRI report should include:
- Patient Information: Name, age, clinical history.
- Technical Details: MRI sequences used, magnet strength (1.5 Tesla), and any contrast agents administered.
- Findings: Detailed description of normal and abnormal structures.
- Conclusion: Summarized impressions and recommendations.
Summary of Key Points
- MRI’s Role: Essential for detailed evaluation of knee structures, aiding in accurate diagnosis.
- Comprehensive Assessment: Enables detection of a wide range of pathologies from traumatic injuries to degenerative conditions.
- Patient Care Impact: Influences treatment decisions and surgical planning.
The Importance of MRI in Patient Care
MRI provides unparalleled soft tissue contrast and multiplanar imaging capabilities, making it invaluable in orthopedic diagnostics. Its use leads to:
- Early Detection: Identifying conditions before they progress.
- Personalized Treatment: Tailoring interventions based on precise findings.
- Improved Outcomes: Enhancing patient recovery and quality of life.
Encouraging Ongoing Learning
The field of MRI is continually evolving with advancements in technology and techniques. Healthcare professionals are encouraged to:
- Stay Updated: Engage in continuous education.
- Collaborate: Work with multidisciplinary teams for comprehensive care.
- Research: Contribute to studies that refine MRI applications.
This guide aims to serve as a valuable resource for understanding the critical role of MRI in evaluating knee pathologies. By integrating anatomical knowledge with practical imaging insights, clinicians can enhance their diagnostic acumen and ultimately improve patient outcomes.
Greater Waterbury Imaging Center offers quality MR imaging services, including orthopedic MR imaging. Contact us for all your MR imaging needs including an orthopedic MRI of the knee.